Abstract
Introduction: Primary central nervous system lymphoma (PCNSL) is a rare subtype of aggressive B-cell lymphoma restricted to the CNS. Despite the use of intensive chemotherapeutic regimens, relapsed or refractory disease (r/r) occurs frequently and depicts a major challenge. Response assessment is usually based on magnetic resonance imaging (MRI), but highly limited due to insufficient discrimination between scar and active tumor tissue. Furthermore, serial biopsies are often not feasible. Accordingly, there is a high unmet medical need for noninvasive risk profiling strategies in PCNSL.
Methods: We applied circulating tumor DNA (ctDNA) sequencing to n=101 blood samples of n=47 patients. Peripheral blood was collected before (pre, n=47), during (mid, n=27) and after (post, n=22) treatment. Sequencing of ctDNA in cerebrospinal fluid (CSF) was performed in 5 patients. Our ctDNA sequencing approach encompasses a targeted gene panel covering >350 genes or genetic regions and an in-house developed bioinformatic pipeline. In the current version, our pipeline shows improved sensitivity and specificity over our previously published version (Sobesky S et al. Med. 2021;2(10):1171-1193.e11), mainly due to the addition of duplex barcode information.
Results: The total amount of cell-free DNA (cfDNA) in plasma was generally low (mean 22.3, range 1.4-208.5 ng/ml) as compared to patients with systemic disease. We hypothesized that cfDNA fragment length profiles and their dynamic changes can inform on outcome in PCNSL as has been recently shown for other lymphomas (Meriranta L et al. Blood. 2022;139(12):1863-1877). To this end, we extracted fragment lengths distributions from all cfDNA samples and used principal component analysis to discern fragment length profiles representative of certain types of samples and remission status. Pre-treatment samples contained higher proportions of short cfDNA fragments (133-173 base pairs (bp)) compared to samples obtained mid-treatment, post-treatment, and healthy controls. In contrast, CSF samples were enriched with ultra-short cfDNA fragments (61-97 bp), which were almost absent in all other samples.
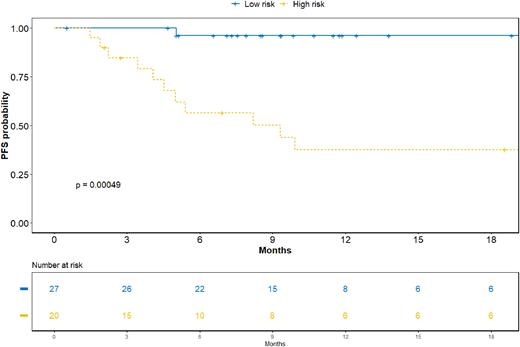
The detection of single nucleotide polymorphisms (SNP) and small insertions or deletions (InDel) was challenging compared to our previously published experience with Hodgkin lymphoma (Sobesky S et al. Med. 2021;2(10):1171-1193.e11). Nevertheless, we detected mutations in most samples, including recurring mutations in PCNSL-associated genes such as MYD88, PIM1 and CD79, though at a lower frequency than expected. The mean baseline ctDNA concentration was 1.7 (range 0-2.8) log haploid genome equivalents (hGE)/ml plasma. Interestingly, the ctDNA concentration was markedly increased in CSF samples. Higher average mutated allele frequency (mAF) in a plasma sample at baseline was associated with reduced progression-free survival (PFS) and overall survival (OS). Patients with a mAF > 1% showed impaired PFS and OS compared to < 1%. No events were observed in patients with mAF < 0.5% (17% of all patients). MRI-based response evaluation indicated partial response in most patients both mid- and post-treatment and thus failed to predict outcomes. Therefore, we assessed mutation-based tracking of peripheral residual disease (PRD). Persistence of PRD during treatment was associated with impaired PFS (median 3.7 vs. 26.9 months, p < 0.0001) and OS (median 4.7 months vs. not reached, p = 0.0009). We hypothesized that dynamic detection of PRD might complement baseline risk stratification by mAF alone. In our final model, baseline low risk patients (mAF low) became high risk when PRD was positive, and baseline high risk patients (mAF high) became low risk when PRD turned negative during treatment. Strikingly, this classification was highly predictive of both PFS (median 9.3 vs. 26.9 months, p = 0.0004, Fig. 1) and OS (median 10.3 months vs. not reached, p = 0.0010).
Conclusions: Surprisingly large differences in fragment length profiles between ctDNA in blood and CSF might yield insight into ctDNA characteristics of both compartments in the context of PCNSL and ctDNA biology in the privileged central nervous system compartment in general. Despite challenges in consistently detecting pathognomonic genetic alterations, assessment of ctDNA-based PRD and fragmentation patterns has the potential to significantly improve treatment guidance in PCNSL patients.
Disclosures
Heger:Novartis: Research Funding; Gilead: Other: Travel support; Incyte: Research Funding. Gödel:Kite/Gilead: Other: Travel Grant. Kutsch:Roche: Honoraria; Janssen: Other: Travel Support; Celgene: Other: Travel Support; Astra Zeneca: Honoraria, Other: Travel support; Gilead Sciences, Inc.: Other: Travel Support, Research Funding. Hallek:Roche, Janssen: Honoraria, Research Funding; Abbvie, AstraZeneca: Consultancy, Honoraria, Research Funding; Bristol Myers Squibb: Consultancy, Honoraria; Gilead: Consultancy, Honoraria. Borchmann:Miltenyi Biotec: Honoraria, Membership on an entity's Board of Directors or advisory committees; Novarts: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; Bristol-Myers Squibb: Honoraria, Membership on an entity's Board of Directors or advisory committees. von Tresckow:Incyte: Consultancy, Honoraria; Allogene: Consultancy; Pfizer: Consultancy; IQVIA: Consultancy; Abbvie: Other: NA; Takeda: Consultancy, Honoraria, Other: NA, Research Funding; Roche: Consultancy, Honoraria, Other: NA; AstraZeneca: Honoraria, Other: NA; Amgen: Consultancy; Miltenyi: Consultancy; MSD: Consultancy, Honoraria, Other: NA, Research Funding; Pentixafarm: Consultancy; Novartis: Consultancy, Honoraria, Other: NA, Research Funding; Gilead/Kite: Consultancy, Honoraria, Other: NA, Research Funding; Cerus: Consultancy; BMS: Honoraria, Other: NA. Borchmann:Liqomics: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees; Galapagos: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal